Military Medicine: Beyond the Battlefield
Episode 1 | 56m 9sVideo has Closed Captions
Bob Woodruff, covers military medical advances from the battlefield to the return home.
ABC News correspondent Bob Woodruff covers military medical advances and technology from the battlefield to the return home. The personal stories of physicians, scientists, active duty troops, veterans, and military families come together in this one hour documentary to show how these advances are both saving and changing the lives of America’s service members.
Problems with Closed Captions? Closed Captioning Feedback
Problems with Closed Captions? Closed Captioning Feedback

Military Medicine: Beyond the Battlefield
Episode 1 | 56m 9sVideo has Closed Captions
ABC News correspondent Bob Woodruff covers military medical advances and technology from the battlefield to the return home. The personal stories of physicians, scientists, active duty troops, veterans, and military families come together in this one hour documentary to show how these advances are both saving and changing the lives of America’s service members.
Problems with Closed Captions? Closed Captioning Feedback
How to Watch Military Medicine
Military Medicine is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipWOODRUFF: From the tragedy of war comes extraordinary advances in medicine.
PADILLA: When I go like that, same thing.
ELSTER: They want to, you know, run that marathon.
They want to ski, they want to a climb a mountain.
WOODRUFF: In the wars since 9/11, the survival rate in combat increased dramatically WOODSON: If war is the dark side of the human experience, medicine has always provided some hope and light.
WOODRUFF: For military medicine, the mission to save lives is also a mission to make lives better.
Till next time.
Yeah.
Now the search is on for the best that science and technology can provide for America's wounded.
This program is made possible by the Corporation for Public Broadcasting as part of Veterans Coming Home, a nationwide public media project helping to bridge the military/civilian divide.
WOODRUFF: Memorials like these across America are dedicated to those who serve in the armed forces, one way we acknowledge their sacrifice and their service.
For those who work in military medicine, that service extends far beyond the war zones, to the survivors, the veterans we honor each November 11.
Now, advances in military medical care saved my life and the life of my ABC News cameraman Doug Vogt when we were injured on assignment in Iraq.
This is the story of the men and women who are winning victories for both military and civilians on this new medical frontier.
This is where medicine meets the needs of the newest generation of America's warriors.
In laboratories and hospitals, from the battlefields to the rehabilitation centers, military medicine is making artificial arms with life-like responses, inventing better tourniquets, 3D-printing new organs, adding robotic arms to wheelchairs, giving damaged legs new strength, and bringing severely wounded troops back from war zones in just a few days.
The goal is not only to save lives, it's to return the wounded to the lives they want to live.
[ Gunfire ] More than 5,300 U.S. military service members were killed in action during the Iraq and Afghanistan conflicts in the years between 2001 and 2014.
SOLDIER: Go!
Come on, come on, come on!
WOODRUFF: But for the thousands of severely wounded who made it to combat hospitals, close to 96% came home alive.
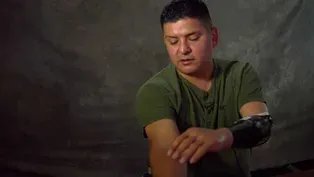
Ramon Padilla is a father and husband, a retired Army sergeant first class who served two tours in Iraq and Afghanistan, and he is the second person in the United States to have this prosthetic arm.
The arm's technology is the first to use implanted sensors to transmit signals to the robotic hand, and its thumb moves, unlike Padilla's older prosthetics.
PADILLA: Before with this hand, I would have to move my thumb over and close it and grip, and now with this one, I don't have to move my thumb over.
I would just power it over and just close it.
WOODRUFF: It's been nine years since Padilla lost his arm and more than 16 years since he volunteered to join the Army.
PADILLA: I was born in Mexico and I got to the States when I was two years old.
So I grew up in Southern California about 13 miles east of downtown L.A.
I had two daughters at an early age, had my high school diploma, and something just clicked where it's like, "Okay, I need to give back, I need to do something.
My family has taken advantage of everything the States has given to us, and -- and I just felt that I had to give back.
WOODRUFF: In May of 2007, Padilla was a staff sergeant with the 173rd Airborne Brigade Combat Team.
He'd already done a tour in Iraq and served seven years in the Army when he was sent to Afghanistan's Korengal Valley.
PADILLA: Well, it was July 8 of 2007.
We just had gotten back from patrol.
Every time I came out of that hooch, I looked up to the mountains, and I looked down -- I looked up at some area that was known for the enemy to be there, all the time, all the time.
I mean, every time I passed through there, I'd look, I'd look, I'd look.
Well, that one time, I didn't look.
Half second later, an RPG blows up next to me.
Shrapnel severs my arm.
I got shot in the right side of the head.
You know, the only time I don't look is where they fire from.
Losing my arm was -- was the least on my mind.
Getting shot on the right side of the head was the least on my mind.
What I cared about the most is the safety of my -- of the warriors that were there with me.
WOODRUFF: Under fire, his team got Padilla out of the valley.
Just six days later, Padilla was on a critical care air transport flight from Germany to the Walter Reed Army Medical Center, where his recovery began with a question for his occupational therapist.
PADILLA: The first thing I asked him, "Look, I want to learn how to play catch with my kid, 'cause I have a lot of fond memories of me and my dad playing catch and teaching me how to play baseball and stuff like that."
Those were lot of special moments in my life I do remember and I wanted to give that to my kids.
Having one arm, I had no idea.
"How the heck am I supposed to do this?"
And he tells me, "We will get you to catch up with your kids."
WOODRUFF: What Padilla and many young wounded warriors wanted was for medical technology to catch up with them.
Padilla now uses a modified lacrosse stick to play catch with his son and a metal grip for golf.
But it started out slowly.
PADILLA: Well, my first hand was my dummy hand, what I call my dummy hand.
So it does not move, does not do anything, it's just a passive hand you put on.
Well, what I wanted was a Luke Skywalker "Star Wars" hand of course, and then later I wanted the "I, Robot" Will Smith hand, and that's the two hands I really wanted, and 'cause you're like, "Oh, my God, this is -- this is in the movies.
Has to be true, right?"
WOODRUFF: Offered a chance to participate in the trial of a robotic arm that would mean having surgery to implant sensors, Padilla was an eager volunteer.
PADILLA: They implanted electrodes inside my muscles, so the same muscles you use to move -- to close your hand, left or right, thumb -- is the same ones I use to power this -- this prosthesis.
So electrodes are in the same muscles.
WOODRUFF: At the Alfred Mann Foundation in Los Angeles, scientists worked with military doctors to design the surgically implanted sensors.
The tiny devices detect signals from existing muscles in the amputated limb, transmit the information wirelessly to the arm's controller, where the signal is translated into commands for the robotic hand and arm to move.
PADILLA: It's slow, of course.
It's not going to be as fast as your hand.
But, as soon as I do it, it happens So whatever your process is from your brain to your muscles to your nerves and however that works, it works.
Go this way.
WOODRUFF: This life-changing technology not only gives Padilla more independence and freedom, it also brings him a step closer to the future he wants for his family and for future generations of wounded troops.
PADILLA: The way I see it is we -- we've got to push technology.
I mean, to me, it's like getting back to that serving again, because even though you may call me a Guinea pig or crash test dummy, whatever you want to call me, all right, I don't care, it's fine.
I'll be that, so that way guys behind me in future wars could have something -- something, when they come back injured, something that's positive, something that will make their lives better.
WOODRUFF: Part of what drives advances in technology is the increasing survival rate in combat.
Men and women with injuries that would have been fatal in earlier wars now make it off the battlefield and back home.
Going to the fixed base.
In 2006, I was severely injured while reporting for ABC News in Iraq.
If it was not for the medical advancements achieved during these most recent wars, I might not have survived.
These videos shot by my brother as I recovered of my wife, my kids, and my family would have looked much different.
Am I lucky?
Look at this.
Because a few months before this, my ABC News team, including my cameraman Doug Vogt, flew to Iraq to cover the war.
Heading up to Camp Taji.
In less than an hour after being struck by an IED, we were flown to a U.S. military hospital in Baghdad to be stabilized.
The only video is this, shot by a soldier on his cell phone.
We were then transferred out of Iraq and on to the Army's Landstuhl Regional Medical Center in Germany.
It was 36 days later when I regained consciousness back in the U.S. at the Navy hospital in Bethesda, Maryland, with my family at my side.
One of the reasons I survived was a dramatic change in how the military brings the wounded home.
During the Vietnam War, travel time for wounded troops from the battlefield back to an advanced care U.S. hospital averaged 45 days.
In the Iraq and Afghanistan conflicts, it dropped to four days.
In my case, it was three days.
My first stop on the way back from Iraq in 2006 was here, the Landstuhl Regional Medical Center in Germany.
Ten years later, I returned to Landstuhl to say thank you and to see what's changed.
LATERZA: Well, you're one of our brothers, you're one of our sons.
WOODRUFF: Colonel James Laterza became Landstuhl's commanding officer in 2015.
WOODRUFF: You know, given the fact that the numbers from the wars have, well, not disappeared but certainly have been reduced, is this place -- it's almost empty compared to the way it was when I was here during that peak time, but if we did not have the kind of training, the kind of size of the -- of the wounded coming in here during that war time, do you think that fewer people's lives would be saved in the civilian medical world that we've got now?
LATERZA: I would have to say yes, and the reason -- the reason being is because of what is learned from large volume of trauma.
And I would say that although the volume of care is lower, the intensity of care, the patients we receive is the same.
We have trauma, it just doesn't happen at the high volume that it happened before.
WOODRUFF: The Landstuhl Regional Medical Center receives wounded and ill service members from throughout the Middle East, Europe, and Africa, but even at the height of the recent wars, it was often a brief stop on the way to a U.S. hospital, usually via nearby Ramstein Air Base.
One of the advances that makes it possible for the severely wounded to get home alive is the creation of critical care air transport teams that turn planes like this C-17 into flying intensive care units.
TIGER: This equipment here, you see that we have our ventilator, our IV pumps, our monitors, our defibrillators, suction canisters.
All normal stuff that you see in a hospital room.
This is how we augment this aircraft for a medical flight.
WOODRUFF: Dr. Michael Tiger, an Air Force major, and his CCATT team were on a rotation from Travis Air Force Base in California.
TIGER: Here we have monitoring equipment.
Specific to CCATT is that our team allows us to minimize the footprint in theater by allowing us to rapidly deploy, evacuate sick patients out of theater, taking them back Stateside or to a higher echelon of care.
WOODRUFF: The advance in critical care transport added up to thousands Of lives saved.
CCATT teams flew more than 5,800 missions, and 99 percent of the patients on board those flights survived.
WOODSON: This was a group that I was training with for critical care aeromedical evacuations.
WOODRUFF: Dr. Jonathan Woodson was the Assistant Secretary of Defense for Health Affairs until May 2016, and deployed as a surgeon in the Army Reserve.
WOODSON: When we began this period of war 15 years ago, we were organized for a Cold War scenario relative to our organization, and of course, with a two-theater war and with the advances in medical care, we had to develop a new system of care throughout this campaign.
And of course, throughout history, through periods of war, there have always been advances in medical care, so if war is the dark side of the human experience, where humanity fails, medicine has always provided some hope and light.
WOODRUFF: For military medicine, it was the enemy's increased use of improvised explosive devices, known as IEDs, in Iraq and Afghanistan that brought about a radical change.
The blasts were designed to kill and maim as many troops as possible, and the resulting injuries meant troops were bleeding to death in minutes.
Trauma medical teams had moved away from using tourniquets, fearing that trying to stem bloodflow would do more harm than good and cause loss or damage of limbs.
But facing IEDs, medics and troops demanded that priority one in trauma care had to be finding a better way to stop bleeding.
COLANTONIO: So this is a CAT tourniquet.
WOODRUFF: Trey Colantonio had this Combat Application Tourniquet, or CAT, when he and the platoon he commanded were in Afghanistan in 2009.
COLANTONIO: And this is -- the principle behind this is to be able to apply it to yourself.
WOODRUFF: It seems simple, but a one-handed tourniquet wasn't in use when Colantonio was accepted to the U.S. Military Academy at West Point in 2004.
COLANTONIO: Put the stick on and basically just crank the stick.
WOODRUFF: At that point, troops were taught a stick and cloth technique that dated back to the Civil War.
COLANTONIO: Yeah, it's a complete change in doctrine from before the wars in Iraq and Afghanistan to now.
Um, you know, going from advise against use of tourniquets to, you know, soldiers on patrol carrying one tourniquet for each extremity and sometimes more than that.
WOODRUFF: The U.S. military says more than one million troops now carry these tourniquets.
Luckily, Colantonio and his troops didn't need them.
All the platoon came home safe.
But once home and promoted to captain, Colantonio wanted to do more for those who were wounded.
Captain Colantonio decided to become Dr. Colantonio.
He applied to what's sometimes called "the best medical school you've never heard of" -- The Uniformed Services University of the Health Sciences in Bethesda, Maryland.
MAN: And then pull out when he's -- WOODRUFF: On its 100-acre wooded campus, U.S.U.
trains both civilians who are commissioned once they enroll and active-duty military service members for military medical careers.
In addition to standard med school training and classes, students here also have to pass field exercises that put them through combat scenarios.
-MAN: All right.
-MAN: Here he comes, -MAN: Coming across.
-MAN: He's all yours.
WOODRUFF: There is a long history of medical lessons learned from combat, but for those who are dedicated to saving lives and caring for the wounded, these advances come at a steep price.
Did you lose any colleagues, any friends?
COLANTONIO: One of my really close friends that we played rugby together, um, was killed in Afghanistan in 2011.
Um...another close friend died in Iraq when I was deployed, um, and then just knowing the quality of men that were over there and suffering these life-changing injuries was really what had an impact on me and made me look towards something that I could do to fix that frustration that I was having, um, about the types of guys that were going over there and not coming home.
MAN: All right.
WOODRUFF: Ramon Padilla admits it's not always easy, but he believes there is no greater generation of warriors when it comes to finding a way forward.
PADILLA: My little boy just made the robotics team, and I made him watch "I, Robot," and I told him, "I want you to make me that hand," and he goes, "Yes, Dad, I'll make you that hand".
PADILLA: I've had some hard times, I've had some bad times, and I've had some great times.
It's not always, you know, roses, you know, blooming.
It's -- you know, you have those times where you're in so much pain, when you just can't wear that prosthesis.
But when you get the opportunity, you know, go ahead and try something new, try something different.
-PASQUINA: Hey.
-PADILLA: Hey, sir.
PASQUINA: Ramon, how are you doing?
-PADILLA: Good, good.
-PASQUINA: Good to see you.
WOODRUFF: Finding ways to make better prosthetics and getting them to wounded warriors like Ramon Padilla is Dr. Paul Pasquina's job.
PASQUINA: You know, right now you've got probably the most advanced motor control than anybody else in the world, um, but you don't have that sensory feedback.
WOODRUFF: Pasquina, a retired Army colonel, is chair of Physical Medicine and Rehabilitation at the Uniformed Services University, and he is the principal investigator for the study of this prosthetic limb.
PASQUINA: As good as that arm is and as much as a leap forward as that is in the technology, it's still not close to what you and I were born with or what they were born with.
WOODRUFF: Restoring a sense of touch is the next step for scientists.
This hand and arm is in development at Case Western Reserve University in Cleveland with funding from the Department of Veterans Affairs and DARPA, the Defense Advanced Research Projects Agency.
PASQUINA: What we hope, and there's already demonstration of this, to be able to put sensors on the tips of the fingers of a prostheses, have those sensors pick up pressure, and then transmit that in an electrical signal back to one's peripheral nerve and have them perceive how much strength of force they're putting through a prosthesis.
WOODRUFF: All of these prosthetics represent progress, but Dr. Pasquina wants to put technology in perspective.
PASQUINA: There's a great deal of celebration about, you know, our ability to save lives on the battlefield, our ability to come up with new and novel technology, but it's that human element that is never replaced by technology.
And, um -- and I guess, you know, I've been doing this long enough to know that despite the advances we've made, there are still many that struggle daily.
I'm always cautious about celebrating too much because there's so much more that needs to be done.
WOODRUFF: You can see science advancing on this new medical frontier in laboratories and hospitals and at universities all across the country.
At the Human Engineering Research Laboratories at the University of Pittsburgh, engineers and designers imagine and manufacture devices that make independent living easier for anyone with a disability.
COOPER: It's easier if you do an open grip on the door, because it comes with you.
MAN: Okay.
WOODRUFF: The laboratories' logo gives the Pittsburgh Panther mascot wheels, because wheelchairs are the main focus.
COOPER: We do wheelchairs and robotics and prosthetics and cognitive AIDS and wireless technologies, virtual reality.
It's here that the labs' director, Rory Cooper, combines his PhD in engineering and his personal experience as a disabled veteran.
Cooper was an Army sergeant stationed in Germany in 1980 when he was hit by a truck while bicycling to his base, leaving him paralyzed below the waist.
Determined to make a difference for all disabled veterans, Cooper decided to study engineering and began building better wheelchairs.
He took up racing, won a bronze medal in the Paralympic Games in 1988, and still competes.
His current challenge -- making wheelchairs with robotic arms.
COOPER: Some people that use wheelchairs, they have limited use of their upper extremities or their arms as well as their legs.
WOODRUFF: The first designs used keyboards and then joysticks to control the arms, and now there's an app for that.
COOPER: So this makes it a lot more intuitive, especially 'cause people are already used to using phones and, um -- and tablets.
I'm just saying up or down, but all the joints are moving in synchrony in order to move me up and down, so the robot's thinking, "Rory wants the bottle to go down," and it's, "What do I -- how do I need to move the joints to do down?"
So in a sense, we're sharing the control.
The robot is doing part of the control and I'm doing part of the control.
So I'll just go up again, and now if you watch, you'll see that the shoulder, the elbow, and the wrists are all moving, so it's doing those calculations.
Instead of having me move every joint and have to do all of that thinking, the robot does some of the thinking for me.
WOODRUFF: To build and manage these complex robots and devices, Cooper makes sure there are veterans and wheelchair-users involved at every level.
COOPER: What we've tried to do is bring all the disciplines together, so physicians and engineers and therapists, and include veterans and people with disabilities and bring them into those professions and use technology to as much as possible ameliorate the disability but also promote full inclusion and full participation in society, and every aspect of society.
SUNDARAM: This is the mobility enhancement robotic wheelchair, or MEBot.
WOODRUFF: Graduate student Andrea Sundaram is working with Cooper on the MEBOT, a powered wheelchair that can keep the seat level while navigating steps or uneven ground.
SUNDARAM: What we tried to do is to make a wheelchair that can go everywhere the current wheelchairs can go and then go places where they can't.
WOODRUFF: The self-leveling chair may mean both better and safer mobility.
SUNDARAM: They had 100,000 reports of emergency room visits by wheelchair users in a single year.
65 to 80 percent of those visits are attributed to tips and falls.
COOPER: It's what happens when you have a war.
Medicine starts sort of at one place and it rapidly has to evolve to another place, um, and for us in rehab, it was the same way.
The trauma surgeons and the -- and the acute care surgeons, they figured how to keep a lot of people alive that wouldn't have normally stayed alive before, and then that gave us in rehab the obligation to help them maximize their function and return to participation.
WOODRUFF: Cooper keeps his own collection of wheelchairs in his office.
COOPER: This is a World War II era chair.
WOODRUFF: It was World War II veterans who first survived spinal cord injuries in large numbers, and as a result, wheelchairs became lighter and more manageable.
COOPER: It was really after World War II that that concept of independence widely became feasible.
WOODRUFF: Cooper says when he saw disabled Iraq and Afghanistan veterans returning home, he knew there was more he had to do.
COOPER: I benefited from what the Vietnam veterans had learned, and then this was kind of the generation that I could -- I was now in a position where I could contribute.
WOODRUFF: Winston-Salem, North Carolina.
In these laboratories at Wake Forest University, scientists have discovered how to grow new human organs and tissues outside the human body.
It's a breakthrough in regenerative medicine.
ATALA: So this is a bio-printed ear scaffold that you see here.
WOODRUFF: Dr. Anthony Atala, the lab's director, and his teams are working on more than two dozen bioengineered tissues and organs and building these kidney, ear, and nose-shaped structures.
ATALA: So this is actually a 3D-printed nose scaffold that we would use basically to recreate the shape as we print these structures.
WOODRUFF: Atala's first scaffold or framework was for a human bladder.
ATALA: We go to the patient and we take a very small piece of tissue from the diseased or injured organ.
We than grow and expand those cells outside the body.
Once we have enough cells for a construct, we create a three-dimensional mold that is shaped like the organ and we place it in an incubator which has the same conditions as a human body.
let it cook, if you will, and then we take it out and implant it surgically back into the patient.
WOODRUFF: So far, Atala has successfully implanted 20 regenerated bladders as part of a clinical trial.
Other organs are not advanced enough for human transplant.
To build more complex organs, researchers here are experimenting with bio-printing.
Instead of ink, cells from a patient are combined with a biodegradable polymer, making a gel-like substance that is slowly layered until a regenerated tissue or organ like this simulated piece of jawbone emerges.
ATALA: Basically when we print these structures, we actually are printing both the cells and the materials together, so then what happens is that the cells themselves start taking over the material, and as the material goes away -- 'cause these are all re-absorbable -- then the cells take over and form the new tissue.
WOODRUFF: The Armed Forces Institute of Regenerative Medicine, established in 2008, funds much of the research here to find new ways to treat battlefield injuries and perhaps to save lives by reducing the need for organ transplants.
ATALA: How can we actually generate new skin?
How can we actually make sure we can cover our wounded warriors that get burns?
All these challenges that appear because of our wounded warriors lead then to studies that aim to replace and regenerate and heal those tissues as much as we can.
At the military's only burn center, in San Antonio, Texas, there are trials underway to test a regenerated skin product called ReCell.
KING: This device can can take a small piece of skin, can dissolve that skin, and convert it into a liquid or a spray.
We collect that into this syringe and then we spray that on a patient.
And, um, the -- skin the size of a postage stamp can cover up that much area on the patient.
WOODRUFF: Dr. Booker King, an Army colonel and director of the burn center, is managing the clinical trial of this spray-on skin.
It's actually not making new skin, but it's causing this -- dissolving the cells and causing the -- when you spray it, the cells will spread out over a greater area.
WOODRUFF: Using this regenerative medicine product could mean fewer skin grafts from the patient's own body.
King says five percent of the wounded in recent wars suffered severe burns KING: These patients need massive resuscitation.
That means they need a massive amount of fluid.
Because of the skin that's injured -- one of the functions of the skin is to maintain your fluid within your body, to regulate that, and also regulate temperature, so because of that injured skin, the patient loses a lot of fluid.
WOODRUFF: To bring burn patients home safely, the Army also deploys burn flight teams.
In 2013, Colonel King and a burn flight team made the longest-ever continuous flight to bring a critically burned patient home.
That patient was Marine lieutenant colonel Brian Forney.
Forney lost his left arm and suffered severe burns when the helicopter he was piloting crashed in Thailand on a training mission.
After surgeries at the burn center, Forney's rehabilitation continued at the Center for the Intrepid.
FERGASON: This all looks great.
Nothing here.
That's never an issue?
-FORNEY: No, that's old.
That used to be an issue all the time, but it hasn't been a problem -- WOODRUFF: Because his burns damaged muscles in his legs and feet, Forney spent almost a year in a wheelchair.
FORNEY: So for a while, there was some question as to whether or not I was going to be able to walk.
I can push down with my right foot, but other than that, my ankles pretty much don't work at all.
WOODRUFF: What gives Forney the strength to stand and walk are these braces invented here called the IDEO, which stands for Intrepid Dynamic Exoskeletal Orthosis.
FERGASON: How long does it take you to get rolling in the morning?
FORNEY: [ Laughs ] Depends on when you start the clock.
From when the alarm goes off, it takes me like half an hour, but if you start from when I actually start moving, it's about 10 to 15 minutes.
Because I've got the IDEO there to give me some rigidity, I can basically lean into it and I can put my force of my weight into this upper cuff, and the strength of the struts on the back keep me upright.
And then when I step, I can load it and it flexes and it allows me to push off.
WOODRUFF: The devices work by storing energy and supporting injured legs and ankles.
FERGASON: Certainly by and large, most of our cases are going to be traumatic war-related kinds of injuries.
If your ankle hurts so bad you can barely function, for most folks, either I have to stop everything I'm doing or I might be considering amputation.
And we've had a lot of people who have considered amputation until they got into this and they've just said, "No, okay, I can work with that.
My pain level now is manageable and I can go on with life again."
[ Whirring ] WOODRUFF: Chief prosthetist John Fergason is in charge of fitting wounded service members with the IDEO and with custom-made artificial limbs.
FERGASON: The biggest thing you'll notice different is that there's no heel cushion, so it just kind of hits and then bounces you forward.
We have an obligation to provide whatever we can to enable someone to get back to a productive life again, and that's not going to change.
These are people in their 20s, they're going to live till whenever, 70, 80, 90, 100 -- God willing, a hundred years old, right, if we want to go that far.
So we have a lot that has to be continually invested to keep folks at the level of activity that they've now been rehabilitated to.
WOODRUFF: A little more than three years after his injury, Lieutenant Colonel Forney returned to duty as the operations officer for a Marine Corps brigade in San Antonio.
FERGASON: Looks like you've had some OT practice.
FORNEY: An IDEO is a pretty expensive piece of gear, but because of the IDEO, I'm going to retire from the Marine Corps, I'm going to be a functioning member of society, I'm going to be able to go get a job, I'm not going to be collecting disability insurance my entire life because I'm stuck in a chair and can't go anywhere and can't do anything.
So it's a big investment, but I think the return on the investment for IDEOs is pretty, pretty massive.
WOODRUFF: Forney is able to have continuing therapy and the IDEO braces because of the Center for the Intrepid's mission.
It was founded with donations from more than 600,000 private citizens during the recent wars, opened in 2007, and was then given to the military.
YANCOSEK: The word "intrepid" means "resolutely courageous," and that's exactly what epitomizes these warriors.
Hi, I'm Lieutenant Colonel Katie Yancosek.
How are you doing?
-MAN: Good, ma'am.
YANCOSEK: Is that your bad hand too?
-MAN: No, this one.
-YANCOSEK: No, okay.
WOODRUFF: Army lieutenant colonel Katie Yancosek is director of the Center for the Intrepid.
YANCOSEK: They want to push the envelope, they want to break the glass ceiling.
If you say this prosthesis only has this much grip and if you continue to do this, this, and this, you're going to break it, then they say, "Well, make me a better arm."
Or they say, "I have to run on a leg.
You have to make me a leg where I can run."
So there's something compelling within them, they have to do it.
They are born to do it, and that warrior spirit doesn't easily subside.
WOODRUFF: Yancosek deployed to Afghanistan, where she was in charge of traumatic brain injury clinics, and she worked with amputees at Walter Reed, specializing in arm and hand rehabilitation.
Her mission now is a combination of those experiences and what the military learned over the past 15 years.
YANCOSEK: We have more insight, so now when we say "polytrauma," it's not necessarily just the list of broken bones and burned flesh and physical wounds, but as important on that list are the kind of unseen wounds and the behavioral, psycho-social things that come along with it.
How can they use their warrior ethos and dedication to duty, selfless service, these types of invisible values that the military emphasizes and maybe not go back to combat, but either remain in service or come into a community and bring all of that too, 'cause you can't amputate that.
So we're much more aware of that now.
[ Gunfire ] WOODRUFF: But by the numbers, the biggest medical challenge for the military is brain injuries.
The Department of Defense estimates that more than 340,000 military service members sustained a traumatic brain injury from mild to severe during the past 15 years, and now there are specialized TBI clinics.
At the Landstuhl Regional Medical Center in Germany, this TBI clinic didn't exist until 2011.
RIVERA: We came to recognize that it's it's not just the moderate or severe, it's not the ones we see.
It's the impact of those that we're not seeing.
-WOODRUFF: The invisible wounds.
-RIVERA: The invisible wounds.
WOODRUFF: Dr. Juan Rivera is the clinic's director.
RIVERA: We also found out the rehab never stops.
So it's not something that after three or four months of rehab, every-- they'll feel better, the patient feels like, "Okay, I can do the things I want to do now.
I can go play golf again, I can load my weapons, I can fire, I can run, I can do things like that."
But the long term impact of that is you need to keep working.
You need to keep those pathways regenerating.
WOODRUFF: Therapists showed me some of the devices that help TBI patients with rehabilitation.
WOMAN: And again.
WOODRUFF: This light board tests vision and helps train reflexes.
Had one in my blind spot.
What is it that we didn't understand before and now we understand?
-RIVERA: Your brain heals.
The brain heals.
The brain recovers.
WOODRUFF: You mean there was an assumption RIVERA: Absolutely.
In neurology, we believe that when the injury is done, the brain was one of the organs that didn't re-generate, that didn't improve its function from the damage, that it was just adaptation.
Other parts of the brain took over and did things that that part that was lost.
What we recognize now is that's not quite the answer.
The answer is the brain actually does repair itself some and actually does recover either from faster pathways or new pathways budding to actually improve that function.
WOODRUFF: That discovery, called neuro-plasticity, is changing lives and treatments, but there is still more unknown than known about brain injuries.
WOODSON: Neuroscience is medicine's Wild West.
It's what we don't -- we know the least about.
The neural circuits, plasticity, potential for repair, drugs to mitigate injury, um, the nexus between actual organic injury and issues like PTSD, um, suicidal ideation later on.
These are all things that we are gaining knowledge about but have vast gaps in our knowledge and need to make progress in.
WOODRUFF: When this began, we didn't really understand much about traumatic brain injury.
That's one that took us a couple years to figure out, this is -- this is horrific and it's -- the numbers are much higher than we ever thought.
WOODSON: And again, that's a consequence of saving individuals who would normally have perhaps bled to death or died from other organ injuries, so now we can focus on the fact that there is this neurological injury and these subtle findings of neurological injury that heretofore had been dismissed as psychiatric issues or other issues.
But as we said before, really it also exposed the great, um, void and gap in knowledge we had about neuroscience to begin with, so part of the reason we didn't address them before is because we had very poor understanding and no strategies for treatment.
DUFFY: Thanks.
WOODRUFF: Watching retired Army sergeant first class Elana Duffy scale this indoor rock wall, you might have trouble seeing the effects of her traumatic brain injury.
DUFFY: I should be a way better climber than I am right now because I've been climbing for 20 years.
But, you know, I can't lift an arm all the way above my head and I can't look down, I can't turn my head a certain way.
WOODRUFF: In 2005, Elana Duffy was serving as an Army intelligence agent in Iraq when an IED hit her convoy on a road outside Baghdad.
DUFFY: It really was targeting the vehicle in front of mine, but they missed, so it ended up going off directly between our two vehicles.
It was maybe 25 meters away.
And I got knocked backwards and my head was positioned directly next to a metal plate that the back of my head slammed into, and even though I had my helmet on, that really does nothing for stopping short that type of momentum.
So I was hit from both ends in quick succession and so I had no idea who anyone was, I didn't really know where I was, I didn't know what was going on.
We ultimately said, like, "No, we'll all continue the mission," because I told everybody I was fine.
WOODRUFF: In the months after, Duffy suffered headaches, vision problems, and memory loss, but she kept her symptoms a secret.
DUFFY: I didn't want to lose my clearance, I didn't want to lose my job, I didn't want to get sent home, I didn't want any of that.
WOODRUFF: What neuroscientists know is that when there is a blow to the head or a nearby concussive blast, the resulting sudden movement causes the brain to move and hit the skull, damaging brain tissue.
Two years after the bomb blast, and by then stationed in Germany, Duffy agreed to see a TBI specialist.
A scan showed there was a bleed in her brain and a tumor.
She had surgery and years of therapy.
She managed to return to duty stateside, but in 2012, Duffy was medically retired from the Army.
DUFFY: TBI is really different from person to person, especially because there are so many different variations of the condition.
It goes from very mild to very severe.
I've met -- there was one TBI guy that like lost almost all speech and lower body -- like lower body movement.
WOODRUFF: Mild TBIs, also known as concussions, might produce headaches and dizziness.
Moderate to severe TBIs may cause balance problems, memory loss, difficulty with language, and depression.
And repeated trauma and severe and penetrating TBIs can cause lasting brain damage.
Duffy says her injury will require rehabilitation for years to come.
DUFFY: I know it holds me back.
I know I'm mentally not where I could be.
I know I'm physically not where I could be.
I still feel like I'm in recovery because I've lost memories and stuff that will never be recovered.
Vertigo, balance issues.
I can't -- I had to go to therapy to be able to walk in a straight line again.
Of course when you're enlisting, you're like, "Oh, yeah, I know that I'm risking my life," but you know that somewhere -- it's -- it's almost like - you're like, "Yeah, but it won't happen to me."
WOODRUFF: The improvised explosive devices that caused the massive increase in brain injuries like Elana Duffy's also meant military medicine had to adopt new strategies for recovery and rehabilitation for a new generation of injured troops.
In 2010, at the height of the war, Dr. Eric Elster, a surgeon and a Navy captain, deployed to Kandahar, Afghanistan.
ELSTER: It was an opportunity for me to go and kind of complete the circle, 'cause I'd been taking care of these casualties at Bethesda for years.
Now I had my opportunity to go to the point of injury.
WOODRUFF: In the six months he was chief of surgery at this combat support hospital, he says the medical teams saw mass casualties almost every week.
ELSTER: We operated on a thousand trauma patients.
We did 3,000 procedures on those thousand patients and we gave 5,000 units of blood, so essentially the business of a major trauma center over a year in six months.
WOODRUFF: The combination of injuries from IEDs meant military medicine had to come up with new systems to save lives.
ELSTER: When we started the wars, there was an Army way, a Navy way, and an Air Force way.
There were discussions between the services, but they were fairly -- you know, fairly isolated in their approaches.
And that's the approach that was, you know, essentially used in World War II, in Vietnam, and in the subsequent years.
So the operational environment pushed us together, pushed us to work together, and we formed what was called the Joint Trauma System, which was a way to ensure that the best care was delivered across a continuum of care, you know, from the point of injury through rehabilitation, because the sooner you get those patients back to, you know, the States, to Walter Reed, to San Antonio or San Diego and the like, the sooner the rehabilitation starts.
WOODRUFF: At home, on hospital rounds at Walter Reed, and as a professor and chair of surgery at the Uniformed Services University, Elster says it's the troops who are the teachers.
ELSTER: The expectations of both the patients but also the health care system was to get patients back to these activities of daily living.
That's not enough for, you know, these men and women.
They want to go back to being, you know, athletes.
They want to, you know, run that marathon, they want to ski, they want to a climb a mountain.
So they're -- they're -- you know, we're pushing them and they're pushing us.
WOODRUFF: What doctors began to see is that rehabilitation worked best when it was veterans helping veterans.
ELSTER: You'll see these soldiers, airmen, Marines working out together, pushing each other.
So I think that's a critical component to the success, is that, you know, again, that ethos, that band of brothers or band of sisters mentality that was so well described by Shakespeare.
MAN: I'm glad y'all are doing so well.
MAN: Oh, thank you, man.
MAN: Light infantry in Vietnam.
'71 to '72.
-BEATTY: Welcome home.
-MAN: Welcome home to you too.
WOODRUFF: Veterans from all branches of the military and from every generation have been coming to Richard's Coffee Shop in Mooresville, North Carolina, for more than 20 years.
MAN: Really good to meet you.
WOODRUFF: Every Thursday, there's free coffee for veterans.
It's a chance to catch up and to connect.
Veterans call it a healing place, and more than 12,000 have stopped by, signed in, and heard "welcome home."
BEATTY: I think this place, Richard's Coffee Shop, is some of the best military medicine around.
[ Applause ] BEATTY: Richard's coffee shop's always great anytime I can go there.
To see so many old friends, and really the best part was when I saw my buddy Lin, who's a World War II vet, and when he said, "I think about you boys every day and what you guys do and I appreciate you."
MAN: Good to see you.
BEATTY: When somebody from the greatest generation tells you you're doing the right thing, then that's what makes my day.
Let's get some coffee.
WOODRUFF: Dale Beatty grew up in a military family in the nearby town of Statesville.
He enlisted in the National Guard right out of high school and was sent to Iraq.
On a routine patrol in 2004, Beatty and his unit, including his friend from home, John Galina, hit an anti-tank land mine on a road outside Baghdad.
BEATTY: I remember pretty much everything.
I was unconscious for about ten seconds.
Woke up, I saw the bottom -- I woke up laying on the ground and saw the bottom of my right boot right here about my knee, so I knew my legs were messed up pretty bad.
Um...it was like one day you're at war with your friends on the battlefield worrying about if you're going to lose your life that day, the next day you're in another country in Germany, the next day you're back in the United States.
WOODRUFF: Beatty's wife Belinda and their two young sons were at his side in the hospital almost as soon as he arrived, and they stayed, living in the Fisher Houses, free lodging provided for military families.
BELINDA: Everything was going to be different.
There was no "the same" anymore.
It was a new normal.
DALE: I was on Ward 57, which is pretty -- pretty famous number for amputees.
I mean, most everybody that came through Walter Reed was on Ward 57, and there were, you know, two, three, four people per room.
So, I mean it was a huge influx of patients and families and, um, very high activity time for the Iraq war and injuries that had happened.
BELINDA: Yeah, I was --- I was quite surprised to see how many were in rooms.
Like, every room was full when I first got to, you know, the hospital.
I just wasn't -- I didn't realize how many were coming home injured like that.
DALE: You want to play?
It's a small town.
I was the only one that got wounded from this local National Guard unit, so it was kind of the story around here.
WOODRUFF: When it was time to come home after a year at the hospital, Dale and Belinda Beatty got some help building a new home.
DALE: And really one of the most I think profound things that affected me was how many other veterans were here all the time working, and it was literally every war from World War II to the Gulf War that were out here volunteering and working on my house.
WOODRUFF: It was the veteran to veteran connection that inspired Beatty along with his friend and fellow guard member John Galina to start Purple Heart Homes.
DALE: We started out Purple Heart Homes just to build a ramp for a veteran, but then realized the -- that psychological impact that we actually had and then knew it was much more than just building homes.
I mean, we were able to maybe not completely do away with but really ease that burden that a lot of these guys had carried around.
WOODRUFF: The organization has spread to other communities and renovated more than 130 veterans' homes.
Ben Wardrip is an Iraq war veteran who lives near Dale Beatty.
WARDRIP: This ramp actually lets me go from inside my house to my vehicle or to the backyard without having to get out of my wheelchair or back into it.
It also allows me easier access to get to my vehicle, to load up and unload.
WOODRUFF: Wardrip suffered a severe back injury and uses a wheelchair most of the day.
He was struggling to manage life with small children in a home with stairs until he asked for help, and Beatty and a team of Purple Heart Homes volunteers with donated supplies showed up and got to work.
WARDRIP: The stress that I had before, the ramp was put in, and before the rails, I didn't -- I didn't ever want to go up my stairs because I'd had like at least four falls, four different falls on stairs within the past year, so it's kind of rough, but at the same time, it's, you know, you kind of have to go up stairs to your bedroom to sleep.
But having the ramp and the stair rails is a big help.
DALE: So, thank our volunteers here and our staff, and most importantly Ben and getting injured, recovering, and establishing a home for you and your family.
Thank you, Ben.
You're welcome, brother.
WOODRUFF: Wardrip and his family and Dale Beatty and his family share lasting issues from their war injuries.
On this day, what they also shared was a bond of service.
DALE: I'll always be honoring and thinking and remembering, because we -- we are a military family, but for those that aren't or don't have a connection, it -- it's not as easy to relate, and I just think that people need to think back.
Who in your family served?
What did they go through?
And if you think about that, most of our country can probably connect to a veteran or to a war at some point in our -- in our nation's history, so we're all connected that way.
WOODRUFF: The science, the technology, and the military medical teams working to save lives hold out great hope for the wounded and their families and for future generations of men and women in the armed services, but there will always be invisible wounds of war, like the one Elana Duffy carries with her.
DUFFY: These are memorial bracelets.
This is for Deyson Cariaga who was killed on the 8th of July in 2005 while I was at the -- sergeant E-5, sergeant promotion board.
He was...20 years old.
He would have turned 21 in like two weeks.
WOODRUFF: The young soldier known as Dice had taken Duffy's place in a convoy that day and was killed when a roadside bomb went off.
DUFFY: I can hardly wrap my own head around it some days.
Um...military people that I talked to who didn't really encounter death in combat, they have trouble comprehending it.
I don't blame anybody for not being able to understand how that weighs on someone.
WOODRUFF: Beyond the battlefield, there is still much to be done and many sacrifices to be remembered.
WOODSON: You know, it goes back to George Washington's phrase, and I paraphrase that now, that the extent to which future generations will serve is directly proportional to how they see the current era veterans being treated, and so if we don't treat them well, if we don't welcome them back into communities and embrace them and fully support them, we put our future national security in jeopardy.
WOODRUFF: Don't let them disappear.
WOODSON: Don't let them disappear.
This program was made possible by the Corporation for Public Broadcasting as part of Veterans Coming Home, a nationwide public media project helping to bridge the military/civilian divide.
Dale Beatty and Battlefield Injuries
Video has Closed Captions
Dale Beatty recounts the moment he was injured on the battlefield. (37s)
Elana Duffy and Treating Traumatic Brain Injury
Video has Closed Captions
Elana Duffy sustained a traumatic brain injury and is still recovering today. (28s)
Lt. Col. Bryan Forney and IDEO Braces
Video has Closed Captions
Severe burns left Lt. Col. Bryan Forney in a wheelchair, but with IDEO braces he can walk. (3m 2s)
Military Medicine: Beyond the Battlefield | Preview
New military medical advances and technology from the battlefield to the return home. (30s)
Ramon Padilla and Cutting-Edge Prosthetics
Video has Closed Captions
Using cutting-edge prosthetics, Ramon Padilla can control his arm with implanted sensors. (32s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipSupport for PBS provided by: